Research project
LOng COvid Multidisciplinary consortium: Optimising Treatments and servIces acrOss the NHS (LOCOMOTION)
- Start date: 1 August 2021
- End date: 31 December 2023
- Funder: National Institute for Health and Care Research (NIHR)
- Value: £3.4m
- Partners and collaborators: ELAROS, Athena CX
- Primary investigator: Dr Manoj Sivan, University of Leeds and Prof Brendan Delaney, Imperial College London
- Co-investigators:
University of Leeds
Prof Rory O’Connor
Prof Daryl O’Connor
Dr Ghazala Mir
Dr Darren Greenwood
Dr Mike Horton
University of Oxford
Prof Trish Greenhalgh
Prof Simon de Lusignan
Prof Stavros Petrou
Imperial College London
Prof Mauricio Barahona
Dr Erik Mayer
Dr Jonathan Clarke
University of Manchester
Dr Alex Casson
Kings College
Dr Vasa Curcin
University of Dundee
Dr Jacqui Morris
University of Exeter
Helen Dawes
Leeds Community Healthcare NHS Trust
Dr Stephen Halpin
Salford Royal NHS Foundation Trust
Prof Nawar Diar Bakerly
Newcastle Upon Tyne NHS Trust
Dr Carlos Echevarria
Oxford University Hospitals NHS Trust
Dr Anton Pick
Oxford Health NHS Foundation Trust
Emma Tucker
Imperial College Healthcare NHS Trust
Dr Sarah Elkin
Birmingham Community Healthcare NHS
Dr Zacc Falope
NHS Wales University Hospital of Wales, Cardiff
Dr Helen Davies
University Hospitals of Leicester NHS Trust
Dr Rachael Evans
Hertfordshire Community NHS Trust
Dr Harsha Master
NHS Highland
Dr Lorna Murray
Patient and Public Involvement (PPI)
Dr Clare Rayner
Prof Ruairidh Milne
Amy Rebane (University of Leeds)
Project Management
Thomas Osborne (University of Leeds)
Madeline Goodwin (University of Leeds)
PDRAs and Clinical Research Fellows
Dr Julie Darbyshire (University of Oxford)
Amy Parkin (Leeds Community Healthcare NHS Trust)
Dr Jordan Mullard (University of Leeds)
Sareeta Baley (Birmingham Community Healthcare NHS Foundation Trust)
Megan Ball (Newcastle NHS Hospitals Foundation Trust)
Joseph Kwon (University of Oxford)
Wenjuan Wang (King's College London)
Dr Samantha Jones (Cardiff and Vale NHS Trust)
Dr Maedeh Mansoubi (University of Exeter)
Johnny Collett (Oxford Brookes University)
Paul Williams (Hertfordshire Community NHS Trust)
Dr Rowena Cooper (NHS Highland)
Kumaran Balasundaram (University Hospitals of Leicester NHS Trust)
Cassie Lee (Imperial College Healthcare NHS Trust)
Rachel Lardner (Oxford Health NHS Foundation Trust)
Vicki Masey (Oxford Health NHS Foundation Trust)
Ana Belen Espinosa-Gonzalez (Imperial College London)
Denise Ross (University of Leeds)
Description
Around two million people in the UK are affected by Long Covid (symptoms persisting for more than four weeks after the first suspected coronavirus (COVID-19) infection that are not explained by something else). Many people still experience issues such as fatigue (extreme tiredness), shortness of breath, muscle ache, changes to thinking skills and loss of smell weeks, months and even over a year after their illness. These symptoms can make daily activities very difficult, especially around the things that are important to people such as caring for loved ones, being able to work or continue to enjoy hobbies.
There are currently 83 Long Covid clinics in England, but we found that waiting times are often long and access is delayed for many people. There is increasing urgency for patients with Long Covid to access prompt, appropriate and efficient care in clinics and doctors’ surgeries, in order to make the best possible recoveries.
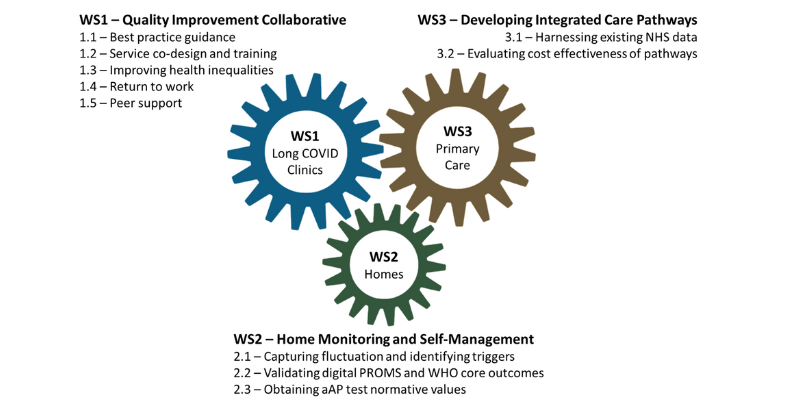
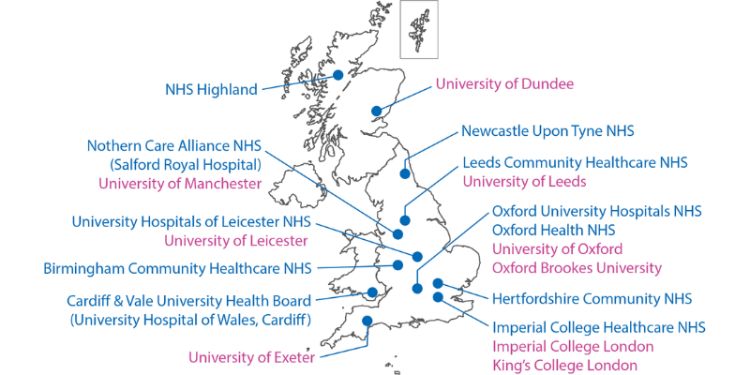
Our research programme will develop a ‘gold standard’ for care by analysing what is happening to patients now, creating new systems of care and evaluating them to establish best practice. This research takes place in ten UK-wide LC clinics treating 5000 patients and involves three parallel workstreams (WS1, WS2 and WS3). Already, by working with health professionals and people with LC, we have found that the key priorities are: correct clinical assessment; advice and treatment; and help with returning to work and other roles.
Workstream 1 (Long Covid clinics) overview:
Workstream 1 involves deriving best practice guidance for Long Covid management by collaborative working between health professionals, patients and researchers from ten NHS clinics. The outputs of this workstream will inform other workstreams for evaluation and adoption of the best practice guidance.
Study 1.1
A Quality Improvement Collaborative (QIC) consisting of Long Covid services from across the UK will share knowledge and learning for best practice management of medical problems, therapy, service model, outcome measures and workforce.
Study 1.2
This experience-based co-design (EBCD) study will link with the QIC and use qualitative interviews with patient and healthcare professional experience to inform the development, improvement and evaluation of patient-centred services.
Study 1.3
This study will examine the inequalities around access and treatment outcomes for different groups of people (in relation to age, sex, ethnicity, pre-existing conditions, disability, socioeconomic circumstances and environmental exposures) to inform Long Covid service improvement and enable equitable care.
Study 1.4
In this study, we will explore the impact of Long Covid on people’s ability to return to work and their ability to fulfil their work roles to develop a Long Covid specific vocational rehabilitation programme which will be tested.
Study 1.5
This study will aim to understand what types of peer support people with Long Covid are utilising in the community, and how peer support groups may be facilitated into wider Long Covid pathways and inform the Quality Improvement Collaborative of study 1.1.
Workstream 2 (Home and self-management) overview:
Workstream 2 involves developing methods for measuring symptoms and functional impact, identifying triggers for the condition, and recording a core set of outcomes.
Study 2.1
This is a two-part study involving the use of wearable technology and daily tasks to gather information about symptoms, daily patterns of symptoms and to identify triggers for worsening of symptoms. This will help to inform health professionals of the best choices of treatment, and help patients self-manage their own symptoms at home.
Study 2.2
A digital platform of core outcome measures will be completed by patients across all ten sites. The core set includes COVID-19 Yorkshire Rehabilitation Scale (C19YRS) which was literature’s first Long Covid scale developed by our research team in Leeds. The scale will be subjected to further validation and Rasch analysis.
Study 2.3
The adapted Autonomic Profile (aAP) is a home-based test of autonomic function that involves measuring blood pressure and heart rate at specific points of the day. Autonomic dysfunction is a common condition in Long Covid patients, and this study will be performing the aAP with ‘healthy’ volunteers to derive normative values for the test.
Workstream 3 (Care models and primary care) overview:
Workstream 3 will use existing data from care of Long Covid patients and the best practice guidance developed in Workstream 1 to develop and evaluate new integrated service care models.
The three workstreams will work in an interdependent and collaborative manner across the ten LC clinics to establish a ‘gold standard’ of treatment and real-time education for healthcare staff and patients that can be shared across the UK.
Impact
Our research will improve access to Long Covid services and establish best practise models of treatment. We know that lack of timely intervention may lead to a longer-term condition if the ‘golden intervention period’ is missed, which is a serious concern for the NHS. Our outputs will standardise care across the four nations and enable the right treatments being delivered to long covid patients in a timely manner. The integrated service care models are likely to influence how care is delivered not only in long covid but across a range of chronic conditions in the future.
Publications and outputs
Support for rehabilitation: self-management after Covid 19 related illness 2nd edition. World Health Organisation (WHO). 2021.
Sivan M, Rayner C, Delaney B. Fresh evidence of the scale and scope of long covid. BMJ. 2021 Apr 1;373:n853.
Parkin A, Davison J, Tarrant R, Ross D, Halpin S, Simms A, Salman R, Sivan M. A multidisciplinary COVID-19 service to manage Post-COVID-19 syndrome in the community. Journal of Primary care and Community Health 2021; 12:1-9
Sivan M, Halpin S, Gee J, Makower S, Parkin A, Ross D, Horton D, O’Connor R. The self-report version and digital format of the COVID-19 Yorkshire Rehabilitation Scale (C19-YRS) for Long Covid or Post-COVID syndrome assessment and monitoring. Advances in Clinical Neurosciences and Rehabilitation 2021 online ahead of print
Sivan M, Halpin SJ, Gee J. Assessing long-term rehabilitation needs in COVID-19 survivors using a telephone screening tool (C19-YRS tool). Advances in Clinical Neurosciences and Rehabilitation 2020; 19: 14‐17
Sivan M, Taylor. NICE guideline on long covid. BMJ 2020; 371:m4938
Halpin S, O’Connor RJ, Sivan M. Long COVID and chronic COVID syndromes. J Med Virol 2020:10.1002/jmv.26587 Halpin SJ, McIvor C, Whyatt G, Adams A, Harvey O, McLean L, Christopher Walshaw C, Kemp S, Corrado J, Singh R, Collins T, Rory J O’Connor RJ, Sivan M. Post-discharge symptoms and rehabilitation needs in survivors of COVID-19 infection: a cross-sectional evaluation. J Med Virol 2021: 93(2): 1013-1022
Sivan M, Halpin S, Hollingworth L, Snook N, Hickman K, Clifton IJ. Development of an integrated rehabilitation pathway for individuals recovering from COVID-19 in the community. J Rehabil Med 2020; 24: 52(8):jrm00089
Patel K, Straudi S, Yee Sien N, Fayed N, Melvin JL, Sivan M. Applying the WHO ICF framework to the outcome measures used in the evaluation of long-term clinical outcomes in coronavirus outbreaks. Int J Environ Res Public Health. 2020; 17(18): E6476.
Sivan M. Remote assessment for identifying COVID-19 post-acute care needs. Aging Clin Exp Res. 2020; 30: 1-2.
Salawu A, Green A, Crooks MG, Brixey N, Ross DH, Sivan M. A proposal for multidisciplinary tele-rehabilitation in the assessment and rehabilitation of COVID-19 survivors. Int J Environ Res Public Health. 2020 Jul 7;17(13):4890.
Ahmed H, Patel K, Greenwood DC, Halpin S, Lewthwaite P, Salawu A, Eyre L, Breen A, O'Connor R, Jones A, Sivan M. Long-term clinical outcomes in survivors of severe acute respiratory syndrome and Middle East respiratory syndrome coronavirus outbreaks after hospitalisation or ICU admission: a systematic review and meta-analysis. J Rehabil Med. 2020 May 31;52(5)
Salawu A, Green A, Crooks MG, Brixley N, Ross DH, Sivan M (2020) A Proposal for Multidisciplinary Tele-Rehabilitation in the Assessment and Rehabilitation of COVID-19 Survivors. International Journal of environmental Research and Public Health. 17, 4890
Sivan M, Halpin S, Gee J, Makower S, Parkin A, Ross D, Horton M, O'Connor R (2021) The self-report version and digital format of the COVID-19 Yorkshire Rehabilitation Scale (C19-YRS) for Long Covid or Post-COVID syndrome assessment and monitoring. Advances in Clinical Neuroscience and rehabilitation
Espinosa-Gonzalez A.B, Master H, Gall N, Halpin S, Rogers N, Greenhalgh T. Orthostatic tachycardia after covid-19. BMJ 2023; 380:e073488.
Jordan M.C.R., Kawalek J, Parkin A, Rayner C, Mir G, Sivan M, Greenhalgh T. Towards evidence-based and inclusive models of peer support for long covid: A hermeneutic systematic review. Social Science & Medicine 2023;115669.
Greenhalgh T, Sivan M, Delaney B, Evans R, Milne R. Long covid - an update for primary care. BMJ 2022;378:e072117.
Sivan M, Greenhalgh T, Darbyshire JL, et al; on behalf of the LOCOMOTION consortium. LOng COvid Multidisciplinary consortium Optimising Treatments and servIces acrOss the NHS (LOCOMOTION): protocol for a mixed-methods study in the UK. BMJ Open 2022;12:e063505.
Sivan M, Greenhalgh T, Milne R, Delaney B. Are vaccines a potential treatment for long covid? BMJ 2022;377 :o988.

