Research project
RESPONSE
- Start date: 1st April 2020
- End date: 30th September 2023
- Partners and collaborators: University of Leeds, Hanoi University of Public Health, Ghana Health Service, University of Ghana, University of Melbourne
Funders: Joint MRC / ESRC / DFID / Wellcome Health Systems Research Initiative
Description
Improving health systems responsiveness to neglected health needs of vulnerable groups in Ghana and Vietnam
Background
The socio-economic growth in many low and middle-income countries (LMICs) has resulted in more available – though not equitably accessible - healthcare. Such growth has also increased demands from citizens for their health systems to be more responsive to their health needs.  Responsiveness, a key goal of any national health system is “…when institutions… are cognisant and respond appropriately to the universally legitimate expectations of individuals... safeguarding of rights of patients to adequate… care” (de Silva, 2000; p.3) and its improvement is the focus of our study.
Responsiveness, a key goal of any national health system is “…when institutions… are cognisant and respond appropriately to the universally legitimate expectations of individuals... safeguarding of rights of patients to adequate… care” (de Silva, 2000; p.3) and its improvement is the focus of our study.
Photo: A family waiting at a hospital reception in Hanoi, Vietnam. © World Health Organization/Sebastian Liste/2018
This study seeks to contribute to improving health systems responsiveness in LMICs through case studies of addressing neglected health needs of vulnerable groups  in Ghana and Vietnam. We will co-produce, implement and evaluate context-sensitive interventions to improve systems responsiveness to the needs and expectations of pregnant women, particularly those with neglected mental health problems.
in Ghana and Vietnam. We will co-produce, implement and evaluate context-sensitive interventions to improve systems responsiveness to the needs and expectations of pregnant women, particularly those with neglected mental health problems.
Photo: Community health workers in Ghana © World Health Organization/Fajan Combrink/2019
Project objectives
Our core question is: “In what way can health systems become more responsive to neglected health needs of vulnerable groups within the contexts of lower-middle-income countries? The project objectives are to:
- Conduct in-depth analyses of how health systems responsiveness is understood and enacted by key health systems actors, and to what degree the local health systems are responsive to these expectations;
- Co-produce, implement and evaluate context-sensitive interventions to improve health systems responsiveness to neglected health needs of vulnerable groups;
- Develop an empirically based and theoretically grounded model of complex relations between the contexts, the mechanisms and the outcomes of the interventions to improve health systems responsiveness;
- Develop transferable best practices for scalability and generalisability of the pilot-tested interventions
- Strengthen research capacity through extending existing collaborations into strong South-South and South-North exchange and learning within and between Ghana, Vietnam, Australia and the UK.
Theoretical framework
We approach health systems responsiveness as a dynamic social action which is produced via relationships between different actors within contexts of particular socio-economic arrangements as they negotiate experiences of professional, citizen, consumer and patient rights and responsibilities.
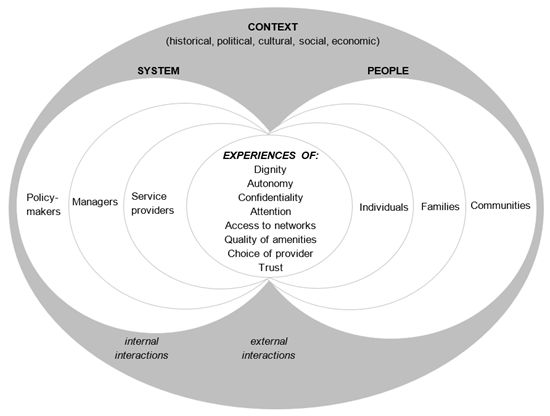
Framework for health systems responsiveness (Adapted from: Mirzoev T and Kane S, BMJ Global Health 2017; 2(4): e000486, Figure 1)
Health systems responsiveness involves two socially-constructed interactions:
- internal (i.e. between policymakers, managers and service providers, for example in resource allocation, target-setting, staff supervision and performance appraisal)
- external (i.e. between people and the system, typically during service provision)
Experiences of these interactions shape degree of health systems responsiveness across its eight domains: dignity, autonomy, confidentiality, attention, access to networks, quality of amenities, choice of service provider and trust. People’s engagements with health systems (e.g. to seek healthcare) and system’s responses to these engagements (e.g. service delivery) are shaped by their initial expectations from each side.
Methods
This theory-driven and mixed methods study will use Realist Evaluation as an overarching methodological framework. Realist researchers develop, test and refine middle-range theories which show causal pathways of how interventions work, for whom and under which conditions. Our initial theory, to be further tested and refined is:
Context-sensitive interventions for better recognition of initial expectations of key actors, if co-produced by these actors to target internal and external interactions and implemented within favourable policy contexts, will improve health systems responsiveness to neglected health needs of vulnerable groups, ultimately contributing to their better health outcomes.
The study comprises three Phases. In Phase 1, we will understand actors’ expectations of responsive health systems, identify key priorities for systems responsiveness, using evidence from the realist synthesis will develop initial programme theory. We will also generate a baseline through reviewing relevant documents and analyse facility records, conduct in-depth interviews, focus groups and community survey.
In Phase 2, we will co-produce the context-sensitive interventions to improve health systems responsiveness. The interventions will seek to improve internal (i.e. within health system) and external (i.e. people-systems) interactions through participatory workshops with health workers and communities, addressing priorities from Phase 1. The co-production will be through meetings with key local, district, regional and national actors, to be led by relevant health authorities and carefully documented by researchers.
In Phase 3, we will implement and evaluate the interventions. The implementation will be through existing structures and processes. In the evaluation, we will test and refine our initial theory through comparing the intended design to the interventions’ actual performance. We will also assess interventions’ feasibility, acceptability and processes.
Outputs and resources
Articles in peer-reviewed journals:
Mirzoev, T., Manzano A., Ha BTT., Agyepong IA., Trang DTH., Danso-Appiah A., Thi LM., Ashinyo ME., Vui LT., Gyimah L., Chi NTQ., Yevoo L., Duong DTT., Awini E., Hicks JP., Cronin de Chavez A., Kane, S. (2021). Realist evaluation to improve health systems responsiveness to neglected health needs of vulnerable groups in Ghana and Vietnam: Study protocol. PLoS ONE, 16(1), e0245755
Protocol registration
Mirzoev T., Manzano A., Cronin de Chavez A., King N., Wright J, Kane S., Agyepong I., Ashinyo ME., Danso-Appiah A., Kretchy I., Gyimah L., Yevoo L., Ha BTT., Trang DTH., Thi LM., Vui LT., Chi NTQ.. Realist synthesis of key strategies to improve health systems responsiveness to health needs of vulnerable groups in low- and middle-income countries. International Prospective Register of systematic reviews (PROSPERO) registration CRD42020200353.
Awareness raising materials
- Project leaflet (English version)
- Project websites at HUPH, University of Melbourne, University of Ghana and Ghana Health Service
Capacity strengthening resources
RealismLeeds Webinar Series 2020 including:
Dr Ana Manzano. Group deliberations (focus groups, etc.) in realist evaluation & realist synthesis.
Joint AMIPS/RESPONSE webinar series on systematic reviews
Impact
Decision-makers from facility, district,  regional and national levels in both Ghana and Vietnam will be continuously engaged through embedding research into policy and practice.
regional and national levels in both Ghana and Vietnam will be continuously engaged through embedding research into policy and practice.
Photo: Health professionals in Ghana © World Health Organization/Fajan Combrink/2019
Key study outcomes and impacts will be: (1) improved health systems responsiveness to neglected health needs of vulnerable groups in Ghana and Vietnam and (2) an empirically-grounded and theoretically-informed model of complex relationships  between the contexts, mechanisms and outcomes of the interventions, along with transferable best practices for scalability (i.e. expansion within similar contexts) and generalisability (i.e. to different contexts, such as other health areas and countries) for future health systems strengthening.
between the contexts, mechanisms and outcomes of the interventions, along with transferable best practices for scalability (i.e. expansion within similar contexts) and generalisability (i.e. to different contexts, such as other health areas and countries) for future health systems strengthening.
Photo: Patients waiting at a clinic in Hoa Binh City in Northern Vietnam © World Health Organization/Sebastian Liste/2018
Project Team
University of Leeds (Nuffield Centre for International Health and Development, Leeds Institute of Health Sciences; School of Sociology and Social Policy)
- Prof Tolib Mirzoev (Principal Investigator)
- Dr Ana Manzano
- Dr Joseph Hicks
- Dr Anna Cronin de Chavez
- Mrs Judy Wright
- Mrs Natalie King
- Ms Alexandra Pisica
- Professor Irene Agyepong (Principal Investigator, Ghana Team Lead)
- Dr Elizabeth Awini
- Ms Linda (Lucy) Yevoo
- Dr Mary Ashinyo
Mental Health Authority, Ghana
Hanoi University of Public Health
- Professor Bui Thi Thu Ha (Principal Investigator, Vietnam Team Lead)
- Dr Do Thi Hanh Trang
- Dr Doan Duong
- Dr Le Minh Thi
- Mrs Quynh Chi Nguyen
- Dr Le Thi Vui
University of Melbourne (Nossal Institute for Global Health, , Melbourne School of Population and Global Health)
- Dr Sumit Kane (Principal investigator)
If you are a researcher, practitioner or policy-maker interested in enhancing responsive health systems, we welcome and invite you to reach out to us.


