Research project
Improving outcomes for chronic orofacial pain including temporomandibular disorders – The TMD study
- Start date: 1 November 2008
- Funder: National Institute for Health and Care Research (NIHR)
- Value: £700,000
- Partners and collaborators: University of Leeds, Manchester University, Leeds Teaching Hospital Trust, Facial Pain Patient and Public Involvement Group
- Primary investigator: Dr Vishal Aggarwal
- Co-investigators: Prof Elspeth Guthrie, Dr Alan Mighell
- External co-investigators: Prof Karina Lovell
Description
The Clinical Problem
Temporomandibular Disorder (TMD) is a collective term for problems affecting the jaw joints and related muscles. Within the musculoskeletal system, the jaw joints have unusual features including the left and right joints working together, the way in which each joint moves and how jaw movement is necessary for activities of day-to-day living such as speaking and eating, which can be impared in people who suffer from TMDs.
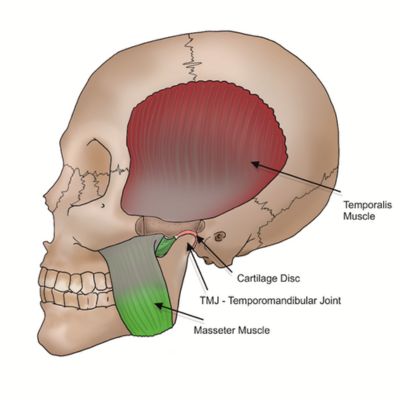
Image of skull with notes to the temporalis muscle at the temple, cartilage disk, TMJ Temporomandibular Joint and Masseter Muscle on the jaw.
Current treatments like mouth guards, pharmacotherapy and / or surgical tooth removal are not supported by Cochrane systematic reviews. These biomedical approaches are directed towards finding and treating an organic pathology for symptoms.
This imposes a huge burden on patients and already stretched healthcare resources. Patients frequently attend multiple specialities in medical and dental settings, where they undergo numerous ineffective and invasive tests and treatments that can be harmful and increase costs to already stretched healthcare services.
Our Solution - Pain Guide Developed in Partnership with Patients
We have developed a self-management pain guide, in partnership with patients who have found the guide helpful for managing their jaw and facial pain.
The Guide can be Downloaded Here
Video to Support the Guide:
Impact
Our pain guide has been implemented in an NHS secondary care settings and improved pain intensity and interference with life, as well as reduced healthcare costs. Remote delivery has positive impact on costs to patient, health service and is environmentally sustainable.
The pain guide was included in the 2018/2019 NIHR annual report that highlights the research achievements that have had the most impact on the UK's health and social care system.
Interventions such as ours are being advocated as first line treatments for temporomandibular disorders TMDs in the National Academies of Medicine TMD report (Link) and Royal College of Surgeon guidelines, currently being published. (Link incoming)
Our systematic review, that provided the evidence base for this treatment, has been cited in national and international guideline and policy documents (NAM report and RCS TMD guidelines, NICE guidance and Wikipedia) which have used this evidence to emphasise that supported self-management should be first line treatment for TMDs and chronic oro-facial pain rather than expensive, irreversible and invasive treatments which have no evidence base and cause harm to the patient.
https://onlinelibrary.wiley.com/doi/10.1002/ejp.1358
Impact on patient quality of life has been substantial. In this patient video, Patient Agata Witkowska explains how TMD has affected her life, and how the guide has helped her manage her condition.
We have also developed a video to enable quick diagnosis of TMDs which demonstrates a quick one minute examination and a red flag checklist for temporomandibular disorders.
Publications and outputs
-
Aggarwal VR, Wu J, Fox F, Howdon D, Guthrie E, Mighell A. 2021. Implementation of biopsychosocial supported self-management for chronic primary oro-facial pain including temporomandibular disorders: A theory, person and evidence-based approach. Journal of Oral Rehabilitation. 48(10), pp. 1118-1128 Link
-
Aggarwal VR, Fu Y, Main CJ, Wu J. 2019. The effectiveness of self-management interventions in adults with chronic orofacial pain: A systematic review, Meta-analysis and Meta-regression. European Journal of Pain. 23(5), pp. 849-865 Link
-
Lovell K, Richards D, Keeley P, Goldthorpe J, Aggarwal V: Self-Management of Chronic Oro-facial Pain including TMD. University of Leeds 2019. Link
-
Goldthorpe J, Lovell K, Peters S, McGowan L, Aggarwal VR. A randomised controlled pilot trial of a guided self-help intervention to manage Chronic Orofacial Pain. J Oral Facial Pain Headache. 2017 Winter;31(1):61-71. doi: 10.11607/ofph.1665. Link
-
Goldthorpe J, Peters S, Lovell K, McGowan L, Aggarwal V. I just wanted someone to tell me it wasn't all in my mind and do something for me": Qualitative exploration of acceptability of a CBT based intervention to manage Chronic Orofacial Pain. British Dental Journal. 2016 May. 220: 459-463 Link

